COVID-19 affects every person differently, but some groups are more at risk than others. As the disease progresses, new research is released, helping scientists understand more about COVID-19 and the expected outcome for certain patients. Due to its novelty, scientists don’t know everything about the coronavirus, but there are certain comorbidities (when a patient has a disease or condition already) and risk factors that have been found to decrease one’s likelihood of surviving COVID-19.
According to the World Health Organization (WHO), the crude mortality rate—the number of deaths divided by the number of cases—is 3 to 4%. If one is over the age of 65, that mortality rate increases, with Intensive Care Unit (ICU) admissions also increasing. Senior citizens make up 80% of reported coronavirus deaths in the United States according to the Center for Disease Control (CDC), making them a high-risk group. The 85+ age group in particular make up around 10% of the US population according to 2010 census data, yet they account for 31% of coronavirus deaths.
Age is a significant risk factor for COVID-19, but individuals with comorbidities such as diabetes, hypertension, cardiovascular disease, obesity (Body Mass Index greater than 30), cancer or immunosuppression also have an increased risk of dying from the coronavirus.
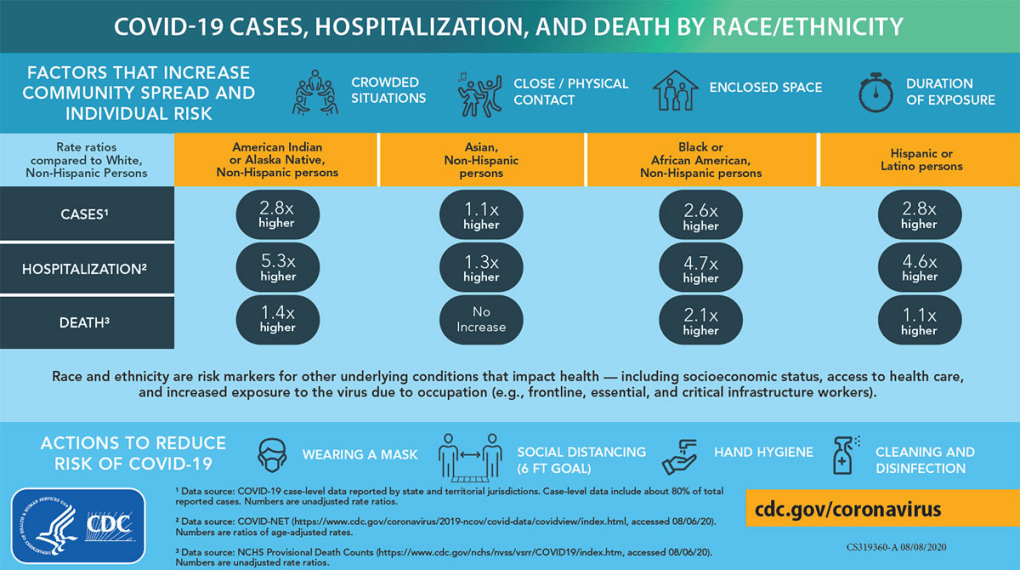
Some risk factors may be less apparent. The CDC found that ethnic minorities, African Americans in particular, are disproportionately affected by the coronavirus. Despite accounting for nearly 18% of coronavirus cases, Non-Hispanic Black Americans make up 13% of the population according to the 2010 census. This is a significant increase, and it could be even larger due to lack of testing in poor, predominantly Black neighborhoods.
Per the CDC, Native Americans are 5.3 times more likely to be hospitalized than white, non-Hispanic individuals. Those of Hispanic or Latino descent are 2.8 times more likely to be diagnosed with the coronavirus. Black Americans are 2.1 times more likely to die from the virus, while there is no increase in death rate of Asian-Americans compared to white Americans. It is unknown whether the increase in cases, hospitalizations and deaths is caused by genetics, high prevalence of poverty, lack of medical resources or, most likely, a combination of the three.
Scientists are discovering possible risk factors constantly. A study claims men are slightly more likely to die from COVID-19 than their same-aged female counterparts. Two other studies suggest that individuals with blood type A have a higher rate of hospitalization while those with blood type O have a slight advantage in surviving the virus. However, all three of these reports use a small sample size, meaning that their findings are not statistically significant and do not play a role in how doctors treat their patients. Scientists will study trends in the future to determine whether biological sex and blood type have an effect on coronavirus outcome.
Ultimately, the student body of American Heritage is young, meaning there is a very low chance of hospitalization due to coronavirus. However, safety precautions such as wearing a mask, social distancing and washing hands can help stop the virus from spreading to high risk individuals. Experts recommend staying vigilant and careful during these trying times.






